Growing the Rural Pharmacy Workforce
UIC's Rural Pharmacy Education program continues filling a state and national void for pharmacists in rural communities
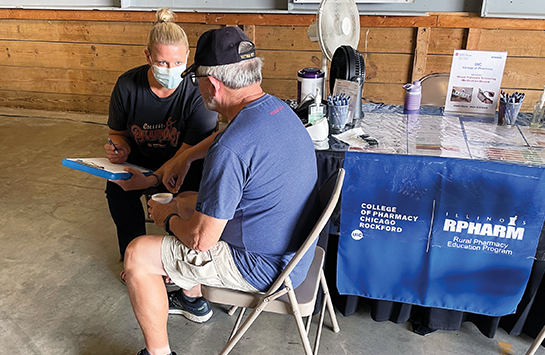
RPHARM

Dr. Elise Wildman’s story begins in Arthur, Illinois, a town of about 2,200 best known for hosting the state’s oldest and largest Amish community—an undeniable nod to its bucolic setting.
There, Wildman remembers visiting Dicks Pharmacy on Vine Street, which featured both an old-time soda fountain and a pharmacist dispensing medications and healthcare guidance. The liveliness of Dicks inspired a young Wildman’s professional ambitions.
“Way back in second grade, I knew I wanted to be a pharmacist,” she says.
To turn that dream into reality, Wildman enrolled in the UIC Retzky College of Pharmacy in 2011, specifically attracted to the Rural Pharmacy Education (RPHARM) program housed at UIC’s Rockford campus. Today, she serves as the inpatient pharmacist at Kirby Medical Center in Monticello, Illinois, a critical access hospital located about 25 miles north of her childhood home in Lovington, one of Arthur’s neighboring towns.
“I love working in a rural community and helping my friends, family, and neighbors,” Wildman says. “Here, I have more face-to-face interaction and an opportunity to work with people on a more personal level that’s really fulfilling.”
Since graduating its first class in 2014, RPHARM— one of only 20 rural pharmacy programs in the United States.—has propelled dozens of pharmacists like Wildman into rural practice and care for underserved populations.
Addressing Needs of Rural Communities
In Illinois, where 65 of the state’s 102 counties are considered rural, pharmacists remain in short supply. Only one in 10 licensed Illinois pharmacists practice in a rural location, according to industry figures, and the dearth of pharmacists in rural communities has been linked to increased rates of hospital readmission and rising health disparities between rural residents and their urban counterparts.
“In many rural communities, pharmacists end up being a first touchpoint, if not a lifeline, because they are the most readily accessible healthcare professional,” says Dr. Kevin Rynn, regional dean for UIC’s Rockford campus. “People come to lean on pharmacists to help them navigate the healthcare arena and receive appropriate care.”
Enter RPHARM, a thoughtfully crafted PharmD concentration preparing students to practice patient-centered, interprofessional pharmacy in rural communities.
UIC launched RPHARM in 2010, the same year the College of Pharmacy established its outpost at the UIC Health Sciences Campus in Rockford. Modeled after the UIC College of Medicine’s longstanding Rural Medicine (RMED) program in Rockford, RPHARM was established to ensure UIC addressed pressing healthcare needs across the state and, in particular, the medically underserved rural areas comprising much of Illinois’s geographic footprint.
“With the RPHARM program, the college committed itself to putting pharmacists in areas with limited healthcare resources and tackling an important patient care void,” says Dr. Allison Schriever, RPHARM’s inaugural director and the current director of pharmacy experiential education on the Rockford campus.
RPHARM imbeds rural-focused course work within UIC’s traditional PharmD curriculum. Over four years, students complete six interprofessional elective courses, three rural healthcare professional shadowing experiences, a community-based research project, and three advanced pharmacy practice experiences in a rural Illinois community. They do much of this alongside students from RMED as well as the UIC College of Nursing’s Rural Nursing (RNURSING) program, an intentional effort to prime students for the interprofessional collaboration rural settings often demand.
“You definitely come to understand the importance of partnerships when working in rural communities because care isn’t so readily available oftentimes,” fourth-year RPHARM student Lauren Johnson says.
Preparing Pharmacy Leaders

Over the last 14 years, RPHARM has successfully prepared a new generation of pharmacists—including some who had never considered rural practice previously—to provide quality services and programs for rural populations. In fact, 40 percent of RPHARM alumni are working in rural environments across 14 states. In Illinois, where the bulk of RPHARM alumni live and work, graduates are serving residents in 19 counties, from Piatt County (population 16,714) in central Illinois to Jo Daviess County (population 21,756) in the state’s northwest corner. The vast majority work in either a community (44 percent) or hospital setting (37 percent), while 11 percent practice in a federal government organization and 6 percent work in a long-term care pharmacy.
“We’re growing our own rural workforce. Students are coming to us for specialized training and returning to help the communities they know and love,” current RPHARM director Dr. Heidi Olson says, adding that more than half of RPHARM alumni practice in communities within 50 miles of their hometowns.
Olson labels RPHARM graduates “a community of doers.” They deliver medications to homes and fill knowledge gaps to ensure medication adherence. They develop outreach programming for schools, community centers, and senior facilities. They partner with the local physical therapist to launch walking groups and collaborate with the neighboring nutritionist to lead healthy eating seminars. They serve on community boards and become preceptors and mentors for others interested in rural pharmacy.
“Our graduates are embedded in their communities and meeting needs far beyond the traditional pharmacist’s role,” Olson says. “They are giving back to their communities by employing things they learned in the program, adapted from others, or developed themselves to cultivate healthier lives and make a difference.”
After working in Centralia, Illinois, for eight years, Wildman joined the Kirby Medical Center team in November 2023 as the hospital’s first-ever full-time inpatient pharmacist. She verifies orders, loads medications, and updates the IV room. Her presence fuels faster, more seamless care for patients, including appropriate medication counseling at discharge.
“I’ve had several patients comment that they’ve never had a pharmacist talk to them in a hospital,” says Wildman, who also oversees medication dispensing machines at two remote clinics.
Johnson, who is slated to graduate in the spring, looks to soon join the ranks of pharmacists practicing in rural communities, where she hopes to promote optimal drug therapy and lead community-based efforts like vaccination clinics or educational outreach at schools.
“I see so much I could do that residents need and will appreciate,” Johnson says.